Antimicrobial Resistance Surveillance in Public Hospitals (2012 - 2017)
Release date: 2 October 2019
Introduction
The HKSAR Government attaches great importance to the threat of antimicrobial resistance (AMR) and has launched the Hong Kong Strategy and Action Plan on Antimicrobial Resistance 2017 - 2022 (Action Plan) in 2017 to combat the problem.
The Action Plan sets out strengthening of AMR surveillance in healthcare settings as one of the strategic actions. It was also suggested in activity 1.2.1 to harmonise AMR surveillance reporting criteria with reference to the Global Antimicrobial Resistance Surveillance System (GLASS), developed by the World Health Organization (WHO). In collaboration with the Hospital Authority (HA), the Department of Health (DH) was provided with laboratory data with antimicrobial susceptibility results of isolated pathogens and demographic data from patients with blood culture specimens for exploration. The scope of data collection includes the six priority pathogens highlighted in GLASS, and respective pathogen-antimicrobial combination of blood culture specimens collected by HA from January 2012 to December 2017.
What is GLASS?
GLASS is developed by WHO to support the Global Action Plan on Antimicrobial Resistance, adopted by the Sixty-eighth World Health Assembly in May 2015.
According to the GLASS Manual for Early Implementation, GLASS is developed in order to echo with one of the five strategic objectives of the Global Action Plan on AMR, which is to strengthen the evidence base through enhanced global surveillance and research. AMR surveillance is the cornerstone for assessing the burden of AMR and for providing the necessary information for action in support of local, national and global strategies.
The goal of GLASS is to enable standardised, comparable and validated data on AMR to be collected, analysed and shared with countries, in order to inform decision-making, drive local, national and regional action and provide the evidence base for action and advocacy. According to WHO, GLASS will initially focus on surveillance data on human priority bacterial pathogens considered the greatest threat globally and progressively incorporate information from other surveillance systems related to AMR in humans, such as foodborne AMR, monitoring of antimicrobial use and surveillance of infections associated with health care. More information about GLASS is available here.
GLASS combines patient, laboratory and epidemiological data to enhance understanding on the extent and impact of AMR. Different priority specimens, pathogens, and pathogen-antimicrobial combinations had been identified. For blood culture specimen, GLASS gathers data on AMR in six priority pathogens identified:
• Escherichia coli
• Klebsiella pneumoniae
• Acinetobacter species
• Staphylococcus aureus
• Salmonella species
• Streptococcus pneumoniae
Methodology and Analysis
With the assistance from various parties of HA, such as Quality and Safety Division, Information Technology & Health Informatics Division, and Special Working Group on AMR, laboratory data and relevant patient data were obtained.
Extracted data were compiled and results were analysed according to the requirements of the GLASS Manual for Early Implementation with local modification. Both positive and negative results were included in the analysis, with the focus of six priority pathogens: Escherichia coli, Klebsiella pneumoniae, Acinetobacter species, Staphylococcus aureus, Salmonella species and Streptococcus pneumoniae.
Specimens are defined as hospital-onset/ community-onset based on the following definition:
- Specimen defined as hospital-onset:
- patient admitted to a health care facility for >2 calendar days, or
- patient admitted to a health care facility for <2 calendar days but transferred from another health care facility where admitted for ≥2 calendar days
- Specimen defined as community-onset:
- patient being cared for at an outpatient clinic when the specimen was taken, or
- patient hospitalised for ≤2 calendar days when the specimen was taken
- When analysing susceptibility results for Salmonella species and Streptococcus pneumoniae, the location of onset was classified as undifferentiated location of onset1
Non-susceptibility results of an antimicrobial derived from less than 10 isolates per year were excluded from analysis.
Antimicrobial susceptibility test results were classified as Susceptible, Intermediate or Resistant. An isolate having susceptibility test result of an antimicrobial being “Intermediate” or “Resistant” is considered as showing non-susceptibility to that drug.
Deduplication was performed according to rules set out by WHO GLASS Manual for Early Implementation, which only one result is reported for each patient per surveyed specimen type and surveyed pathogen for each surveillance period (i.e. every 12 months).
When interpreting the antimicrobial susceptibility test results, readers are cautioned that they should also take into consideration of the number of isolates that have the susceptibility test results of concerned.
Key Findings
Patient characteristics
It was observed that blood culture specimens were more commonly collected among patients aged 65 or above. Number of patients with blood culture specimen collected increased from 123,026 in year 2012 to 158,749 in year 2017. Percentage of patients with positive blood culture ranged from 10.08% in 2017 to 11.10% in 2015.
General Results
In year 2017, 41.21% of patients with positive blood culture had Escherichia coli isolated, followed by Klebsiella pneumoniae (11.65%) and Staphylococcus aureus (10.62%).
Generally speaking, among blood culture specimens collected in public hospitals, the percentages of non-susceptibility on majority of selected antimicrobials for the six WHO GLASS priority pathogens remained stable or with slight decreasing trend during the surveillance period. However, increasing trends were also observed among several drug-bug combinations that might warrant further investigation and monitoring. The key results of the six targeted pathogens were presented in the ensuing paragraphs.
Equation for calculating percentage values in the ensuing paragraphs is as below:
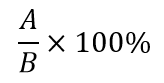
A: No. of patients with bacteria X isolated from blood culture, and bacteria X showed non-susceptibility to drug Y
B: No. of patients with bacteria X isolated from blood culture
Escherichia coli
For isolates of Escherichia coli, percentages of non-susceptibility were lower among isolates of community-onset than those of hospital-onset. Trends of non-susceptibility remained stable2 for many commonly used antimicrobials treating Escherichia coli infections, with decreasing trends observed towards amoxicillin/ clavulanate (range: 26.35% (Year 2017) - 32.52% (Year 2013)), gentamicin (range: 28.28% (Year 2017) - 31.16% (Year 2012)) and amikacin (range: 0.42% (Year 2017) - 1.35% (Year 2013)) among community-onset isolates, and amoxicillin/ clavulanate (range: 38.32% (Year 2017) - 47.11% (Year 2013)), cefuroxime (range: 38.41% (Year 2017) - 48.64% (Year 2012)), cefotaxime (range: 35.59% (Year 2017) - 44.41% (Year 2012)) and levofloxacin (range: 39.47% (Year 2017) - 49.67% (Year 2013)) among hospital-onset isolates. Increasing trend of non-susceptibility to cefepime3 (range: 12.46% (Year 2013) - 24.05% (Year 2015)) among community-onset isolates warranted further monitoring and deliberation for using the drug as empirical therapy for treating severe Escherichia coli infection. Non-susceptibility of carbapenems remained low and stable4.
Klebsiella pneumoniae
For isolates of Klebsiella pneumoniae, similar pattern comparable with that of Escherichia coli was noted. The percentages of non-susceptibility were lower among isolates of community-onset than those of hospital-onset. Trends of non-susceptibility were stable5 among commonly used beta-lactam/ beta-lactamase inhibitor combinations, including amoxicillin/ clavulanate and piperacillin/ tazobactam, as well as major parenteral second- and third-generation cephalosporins, for isolates of both community-onset and hospital-onset, with an exception that an increasing trend was observed for cefotaxime non-susceptibility among isolates of hospital-onset (range: 25.00% (Year 2013) - 35.37% (Year 2016)). Non-susceptibility of carbapenems remained low during the period. Increasing trend of non-susceptibility to cefepime6 among isolates of community-onset (range: 4.76% (Year 2012) - 8.40% (Year 2016)) and hospital-onset (range: 9.25% (Year 2013) - 22.15% (Year 2017)), and that of ciprofloxacin (range: 18.42% (Year 2012) - 42.67% (Year 2016)) and levofloxacin (range: 12.76% (Year 2012) - 22.80% (Year 2017)) among hospital-onset isolates warranted further monitoring.
Staphylococcus aureus
For isolates of Staphylococcus aureus, community-onset isolates reported a lower non-susceptibility percentage to oxacillin than those of hospital-onset. Trend of non-susceptibility percentage to oxacillin remained stable7 during the period for both isolates of hospital-onset (range: 53.11% (Year 2012) - 59.97% (Year 2016)) and community-onset (range: 35.65% (Year 2012) - 40.26% (Year 2016)). Non-susceptibility of vancomycin reported as less than 0.005% during the surveillance period.
Salmonella species
For undifferentiated8 isolates of Salmonella species, which is a pathogen primarily causing community-acquired infections, increasing trends of non-susceptibility percentage to fluoroquinolones (ciprofloxacin9 range: 51.88% (Year 2012) - 76.39% (Year 2017), levofloxacin10 range: <0.005% (Year 2013) - 86.36% (Year 2017) and ampicillin range: 35.03% (Year 2012) - 62.44% (Year 2016)) were observed11. Trends of non-susceptibility percentage to third-generation cephalosporins remained stable12, with non-susceptibility percentage at 5.18% for ceftriaxone in 2017. Non-susceptibility of carbapenems remained at less than 0.005% during the period.
Acinetobacter species
For isolates of Acinetobacter species, community-onset isolates generally showed a lower non-susceptibility percentage than those of hospital-onset. For hospital-onset isolates, decreasing trends of non-susceptibility percentage to gentamicin (range: 26.17% (Year 2017) - 50.34% (Year 2013)) and minocycline (range: 28.89% (Year 2017) - 75.00% (Year 2012)) were observed, non-susceptibility trends among major groups of antimicrobials, including beta-lactam penicillins, cephalosporins, carbapenems13, fluoroquinolones and aminoglycosides remained stable14.
Streptococcus pneumoniae
For undifferentiated15 isolates of Streptococcus pneumoniae, trends of non-susceptibility percentage to penicillin (range: 0.66% (Year 2015) - 1.96% (Year 2017)), cefotaxime (range: 0.89% (Year 2017) - 7.63% (Year 2015)), ceftriaxone (range: 1.16% (Year 2015) - 7.23% (Year 2013)) and levofloxacin (range: <0.005% (Year 2012) - 1.34% (Year 2017)) remained stable16. Non-susceptibility percentage of erythromycin remained high (range: 69.53% (Year 2012) - 80.56% (Year 2014)). An increasing trend of non-susceptibility percentage to sulfamethoxazole/ trimethoprim (range: 46.98% (Year 2013) - 70.00% (Year 2017)) was observed during the period.
Discussion
This exercise contributed to the understanding of AMR situation in Hong Kong. Among blood culture specimens collected in public hospitals in Year 2012 to 2017, the percentages of non-susceptibility on majority of selected antimicrobials for the six WHO GLASS priority pathogens remained stable or with slight decreasing trend during the surveillance period. Yet, increasing trends were observed among several drug-bug combinations that might warrant further investigations and monitoring.
Nevertheless, readers should bear in mind that AMR remains a major threat in the world and Hong Kong is of no exception. From the results, high non-susceptibility percentages in conventionally used antimicrobials among some common pathogens were observed, such as oxacillin non-susceptibility among Staphylococcus aureus and ceftriaxone/ cefotaxime non-susceptibility among Escherichia coli and Klebsiella pneumoniae, which renders some of the first-line antimicrobials ineffective in treating infections caused by these pathogens. In addition, some of the non-susceptibility figures were higher when compared with that of overseas countries, e.g. proportion of Staphylococcus aureus being oxacillin-resistant in UK is lower than that of Hong Kong17. As such, concerted efforts of different parties, including the prudent antimicrobial use and comprehensive infection prevention and control strategies, are the key measures to combat AMR.
Bear in mind that AMR remains a major threat in the world including Hong Kong, members of the public and healthcare workers are reminded of the following advice to combat AMR:
Advice to the Public
- Proper use of antibiotics
- Do not demand antibiotics from your doctor
- Follow your doctor’s advice when taking antibiotics
- Do not stop taking antibiotics by yourselves even if you are feeling better
- Do not take leftover antibiotics
- Do not share your antibiotics with others
- Do not self-purchase antibiotics without a prescription
- Practise frequent hand hygiene, especially before eating and taking medicine, and after going to the toilet
- Ensure your vaccination is up-to-date
- Maintain cough etiquette, wear a surgical mask if you have respiratory symptoms
Advice to Healthcare Workers
Antimicrobials are a precious resource and their effectiveness must be preserved to protect us from infections. Healthcare workers play an essential role in preserving them:
- Prescribe antibiotics in accordance with therapeutic guidelines in consideration of clinical situations
- Educate your patients
- To take antibiotics as prescribed and always complete the full course of medication
- Discuss about the importance of appropriate antibiotic use and the dangers of AMR where appropriate
- Talk about how to prevent infections and their spread. For example, vaccination, maintain good personal hygiene and hand hygiene
- Apply best practice of infection prevention and control, and to practise frequent hand hygiene
- Receive seasonal influenza vaccine
Please click here to view the more detailed results.
Please click here to view the full report.
1 Salmonella species and Streptococcus pneumoniae are pathogens primarily causing community-acquired infections. They are rare to cause hospital-associated infections. Information on location of onset is not considered when analysing and interpreting non-susceptibility results of these two pathogens. These results will be interpreted as isolates of onset of unknown location.
2 No statistically significant upward/ downward trend was observed.
3 Readers should take note that a new (revised) cefepime interpretive criteria for Enterobacteriaceae was released by the Clinical & Laboratory Standards Institute (CLSI) in 2014, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility.
4 No statistically significant upward/ downward trend was observed.
5 No statistically significant upward/ downward trend was observed.
6 Readers should take note that a new (revised) cefepime interpretive criteria for Enterobacteriaceae was released by CLSI in 2014, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility.
7 No statistically significant upward/ downward trend was observed.
8 Salmonella species and Streptococcus pneumoniae are pathogens primarily causing community-acquired infections. They are rare to cause hospital-associated infections. Information on location of onset is not considered when analysing and interpreting non-susceptibility results of these two pathogens. These results will be interpreted as isolates of onset of unknown location.
9 Readers should take note that a new ciprofloxacin interpretive criteria for Salmonella species was released in 2012 and modified recommendations to use separate ciprofloxacin interpretive criteria for Salmonella species was released in 2013 by CLSI respectively, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility.
10 Readers should take note that a new levofloxacin interpretive criteria for Salmonella species was released by CLSI in 2013, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility.
11 Readers are cautioned when interpreting the non-susceptibility percentage to levofloxacin in particular as the percentage is calculated based on the susceptibility test results from a relative few isolates.
12 No statistically significant upward/ downward trend was observed.
13 Readers should take note that a new (revised) imipenem and meropenem interpretive criteria was released by CLSI in 2014, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility.
14 No statistically significant upward/ downward trend was observed.
15 Salmonella species and Streptococcus pneumoniae are pathogens primarily causing community-acquired infections. They are rare to cause hospital-associated infections. Information on location of onset is not considered when analysing and interpreting non-susceptibility results of these two pathogens. These results will be interpreted as isolates of onset of unknown location.
16 No statistically significant upward/ downward trend was observed.
17 Please click here to access the English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report.