Knowledge, Attitude and Practice Survey of Medical Practitioners on Antimicrobial Resistance 2019
Release date: 30 October 2020
Knowledge, Attitude and Practice Survey of Medical Practitioners on Antimicrobial Resistance 2019
Introduction
The Department of Health (DH) commissioned a research centre to conduct a knowledge, attitude and practice (KAP) survey of medical practitioners on antimicrobial resistance (AMR) (“the Survey”) in 2019.
Survey method
The sampling frame of the Survey involved a random sample of medical practitioners with full registration with the Medical Council of Hong Kong under the Medical Registration Ordinance who were on the Resident List of the General Register as at 1 July 2018. The Survey was conducted by self-administrated paper-based or web-based questionnaire consisting of 24 questions in English. Paper-based questionnaires with unique QR code and password (for access to web-based questionnaire) were mailed to selected medical practitioners. The fieldwork was conducted during 11 September to 31 December 2019, achieving a sample size of 1 074 (including 364 primary care doctors) and a response rate of 12.3%.
Key findings relevant to members of the public and patients
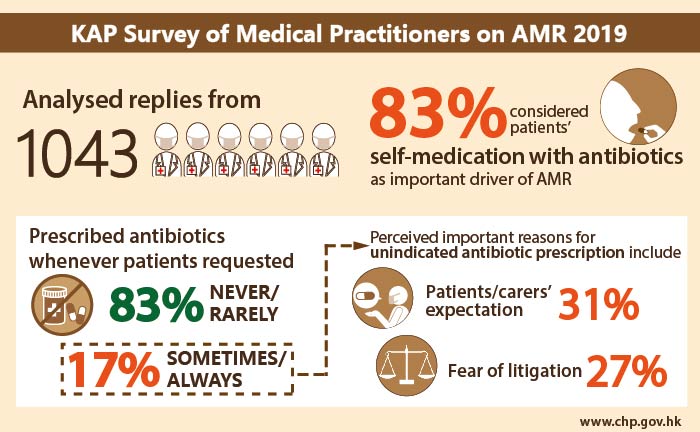
- Findings of the Survey were based on the 1 043 medical practitioners who were practising in Hong Kong as of 30 June 2019. Respondents considered that patients’ self-medication with antibiotics (83.3%) and inappropriate choice of drug (83.0%) were important drivers of AMR.
- More than half (59.4%) of the respondents were “always”/“often”/“sometimes” requested by patients for antibiotics for cold/flu/upper respiratory tract infection (URTI), and higher frequency of such requests were associated with doctors who were male or in the general practice field. Despite this, a majority (83.0%) of all respondents "rarely"/"never" prescribed antibiotics whenever patients requested.
- “Uncertain clinical diagnosis” was considered by the highest proportion (56.0%) of respondents to be an important (“very important”/“slightly important”) reason for unindicated antibiotic prescription, followed by “expectation/request of antibiotics by patients or carers” (23.8%) and “cannot ensure return of patient for follow up” (17.7%).
- The frequency of prescribing antibiotics for uncomplicated URTI whenever patients requested was significantly associated with the perceived importance of reasons for unindicated antibiotic prescription including patients/carers’ expectation or request, being unable to ensure the return of patient for follow up, no time to explain why not indicated and fear of patient’s litigation. Among those reported "always"/"often"/"sometimes" prescribed antibiotics for uncomplicated URTI whenever patient requested, 30.9% and 26.9% considered “expectation/request of antibiotics by patients or carers” and “fear of patient’s litigation” respectively as important reasons accounting for unindicated antibiotic prescription and these proportions were significantly lower among those reported “rarely”/“never” (less than 25% and 15% respectively).
Recommendations relevant to members of the public and patients
Since patients’ self-medication with antibiotics was considered by most respondents an important driver of AMR, members of the public should be explained more about the disastrous consequences of AMR instead of merely asking them to stop practicing self-medication.
With significantly more respondents who "always"/"often"/"sometimes" prescribed antibiotics for uncomplicated URTI upon patients’ requests considered “expectation/request of antibiotics by patients or carers” and “fear of patient’s litigation” as important reasons of unindicated antibiotic prescription, and a significant proportion of respondents were frequently requested by patients for antibiotics for cold/flu/URTI, patient education and expectation management should be enhanced in public promotional campaign.
The executive summary and the full report can be accessed here.