Antimicrobial Resistance Surveillance in Public Hospitals (2018)
Release date: 15 January 2021
Introduction
The HKSAR Government attaches great importance to the threat of antimicrobial resistance (AMR) and has launched the Hong Kong Strategy and Action Plan on Antimicrobial Resistance 2017-2022 (Action Plan) in 2017 to combat the problem.
The Action Plan sets out strengthening of AMR surveillance in healthcare settings as one of the strategic actions. It was also suggested in activity 1.2.1 to harmonise AMR surveillance reporting criteria with reference to the Global Antimicrobial Resistance Surveillance System (GLASS), developed by the World Health Organization (WHO). In collaboration with the Hospital Authority (HA), the Department of Health (DH) was provided with laboratory data with antimicrobial susceptibility results of isolated pathogens and demographic data from patients with blood culture specimens for analysis. The first Summary Report on Antimicrobial Resistance Surveillance in Public Hospitals (2012-2017) taking reference to the Global Antimicrobial Resistance Surveillance System (GLASS) from the World Health Organization (WHO) was published in October 2019 at the website of the Centre of Health Protection (CHP) of DH.
To continue with this surveillance activity, DH analysed the data for year 2018 provided by HA and prepared this report. The scope of data collection includes the six priority pathogens highlighted in GLASS, and respective pathogen-antimicrobial combination of blood culture specimens collected by HA from January 2012 to December 2018.
What is GLASS?
GLASS is developed by WHO to support the Global Action Plan on Antimicrobial Resistance, adopted by the Sixty-eighth World Health Assembly in May 2015.
According to the GLASS Manual for Early Implementation, GLASS is developed in order to echo with one of the five strategic objectives of the Global Action Plan on AMR, which is to strengthen the evidence base through enhanced global surveillance and research. AMR surveillance is the cornerstone for assessing the burden of AMR and for providing the necessary information for action in support of local, national and global strategies.
The goal of GLASS is to enable standardised, comparable and validated data on AMR to be collected, analysed and shared with countries, in order to inform decision-making, drive local, national and regional action and provide the evidence base for action and advocacy. According to WHO, GLASS will initially focus on surveillance data on human priority bacterial pathogens considered the greatest threat globally and progressively incorporate information from other surveillance systems related to AMR in humans, such as foodborne AMR, monitoring of antimicrobial use and surveillance of infections associated with health care. More information about GLASS is available here.
GLASS combines patient, laboratory and epidemiological data to enhance understanding on the extent and impact of AMR. Different priority specimens, pathogens, and pathogen-antimicrobial combinations had been identified. For blood culture specimen, GLASS gathers data on AMR in six priority pathogens identified:
- Escherichia coli (E. coli)
- Klebsiella pneumoniae (K. pneumoniae)
- Acinetobacter species (Acinetobacter spp.)
- Staphylococcus aureus (S. aureus)
- Salmonella species (Salmonella spp.)
- Streptococcus pneumoniae (S. pneumoniae)
Methodology and Analysis
With the assistance of stakeholders from HA such as Information Technology & Health Informatics Division, Quality and Safety Division, Strategy and Planning Division, and various Working Groups, laboratory data and relevant patient data were obtained.
Extracted data were compiled and results were analysed according to the requirements of the GLASS Manual for Early Implementation with local modification. Both positive and negative results were included in the analysis, with the focus of six priority pathogens: Escherichia coli, Klebsiella pneumoniae, Acinetobacter species, Staphylococcus aureus, Salmonella species and Streptococcus pneumoniae.
Specimens are defined as hospital-onset/community-onset based on the following definition:
- Community-onset (CO) specimen/isolate:
- Hospital-onset (HO) specimen/isolate:
- When analysing susceptibility results for Salmonella species and Streptococcus pneumoniae, the location of onset was classified as undifferentiated location of onset[5]
Non-susceptibility results of an antimicrobial derived from less than 10 isolates per year were excluded from analysis to avoid biased results.
Antimicrobial susceptibility test results were classified as Susceptible (S), Intermediate (I) or Resistant (R). An isolate having susceptibility test result of an antimicrobial being “Intermediate” or “Resistant” is considered as showing non-susceptibility to that drug.
Non-duplicated isolates of WHO GLASS priority organism from each patients were included based on the WHO GLASS Manual for Early Implementation with local adaptation.
When interpreting the antimicrobial susceptibility test results, readers are cautioned that they should also take into consideration of the number of isolates that have the susceptibility test results of concerned.
Key Findings
Patient characteristics
During the surveillance period, total number of patients with blood culture specimen collected was on the rise from 123,000[6] in year 2012 to 159,000[7] in year 2018. Over half of those specimens were collected among patients aged 65 or above.
The annual blood culture positive rate during the surveillance period ranged from 10.1% to 11.1%. Patients aged 65 or above had the highest positive rate for blood culture specimen of community-onset (CO), hospital-onset (HO) and undifferentiated location of onset (UO).
Overview of culture test result
Distribution of patients with these organisms isolated from blood culture specimen remained similar. In year 2018, the three commonest WHO GLASS priority organisms were Escherichia coli (CO: 46.4%; HO: 24.8%), Klebsiella pneumoniae (CO: 11.6%; HO: 10.3%) and Staphylococcus aureus (CO: 8.4%; HO: 17.9%).
Generally speaking, among blood culture specimens collected in public hospitals, the non-susceptibility percentages on majority of different antimicrobials for the six WHO GLASS priority organisms remained stable or with slight decreasing trends during the surveillance period. However, increasing trends of non-susceptibility percentage were also observed among several pathogen-antimicrobial combinations that may warrant further monitoring. The key results of the six targeted pathogens were presented in the ensuing paragraphs. All trends on non-susceptibility percentage mentioned here imply the presence of statistical significance, and are referring to the period of year 2012-2018 unless otherwise specified.
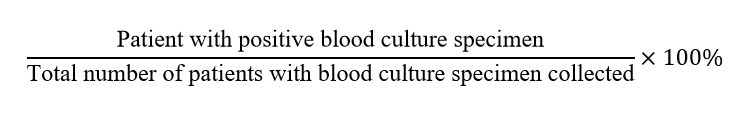
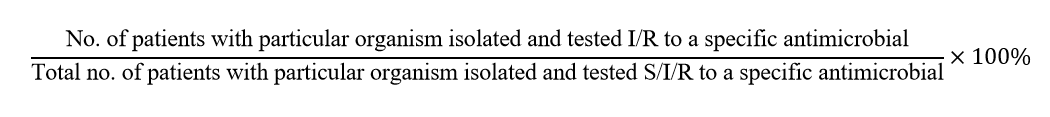
Definitions and formulas used in the ensuing paragraphs on percentages are listed as below:
- Positive percentage/rate
- Non-susceptibility percentage/rate
Escherichia coli
In general, non-susceptibility percentages on different antimicrobials were lower among E. coli isolates of community-onset than those of hospital-onset. Decreasing trends with statistical significance were observed for amoxicillin/clavulanate[8],[9], piperacillin/tazobactam[10],[11], gentamicin[12],[13] and amikacin[14],[15] among the isolates of both community- and hospital-onset, and cefuroxime[16], cefotaxime[17], ceftazidime[18] and levofloxacin[19] among isolates of hospital-onset. Non-susceptibility percentage for cefepime[20],[21] showed an increasing trend with statistical significance for isolates of community-onset, but such trend was not observed for isolates of hospital-onset. When adopting year 2016 data as the baseline, a decreasing trend with statistical significance was observed for piperacillin/tazobactam for isolates of both community- and hospital-onset, while trends on non-susceptibility percentage of antimicrobials above-mentioned remained stable.
Klebsiella pneumoniae
Non-susceptibility percentages on different antimicrobials were generally lower among K. pneumoniae isolates of community-onset than those of hospital-onset. Increasing trends with statistical significance were observed for ciprofloxacin[22] and levofloxacin[23] for isolates of hospital-onset, and cefepime[24],[25],[26] for isolates of both community- and hospital-onset. When adopting year 2016 data as the baseline, trends on non-susceptibility percentage of antimicrobial above-mentioned remained stable. For carbapenems, the non-susceptibility percentages showed a significant increase from less than one percent in year 2017 to more than three percent in year 2018 for both imipenem[27] and meropenem[28] for isolates from hospital-onset specimens.
Staphylococcus aureus
Non-susceptibility percentage on oxacillin was higher among S. aureus isolates of hospital-onset than those of community-onset. Trend on non-susceptibility for oxacillin remained stable during the period of year 2012-2018 and 2016-2018. None of the tested isolates were non-susceptible towards vancomycin.
Salmonella species
Non-susceptibility percentage for ampicillin[29], ciprofloxacin[30],[31] and levofloxacin[32],[33] showed increasing trends with statistical significance from year 2012 to 2018. These trends were not observed when year 2016 data was adopted as the baseline.
Acinetobacter species
Non-susceptibility percentages on different antimicrobials were generally lower among Acinetobacter spp. isolates of community-onset than those of hospital-onset from year 2012 to 2018. Decreasing trends with statistical significance were observed for minocycline[34], gentamicin[35] and amikacin[36] for isolates of hospital-onset. When adopting year2016 data as the baseline, trends on non-susceptibility percentage of antimicrobial above-mentioned remained stable for isolates of both community- and hospital-onset.
Streptococcus pneumoniae
Non-susceptibility percentages for co-trimoxazole[37] showed an increasing trend with statistical significance from year 2012 to 2018. The trend was not observed when year 2016 data was adopted as the baseline.
Discussion and Conclusion
Among blood culture specimens collected from year 2012 to 2018, non-susceptibility percentages on majority of different antimicrobials for the six WHO GLASS priority organisms remained stable or with a slight decreasing trend during the surveillance period.
However, increasing trends were observed among several pathogen-antimicrobial combinations. In particular, trends of non-susceptibility percentages for carbapenems among Klebsiella pneumoniae warrant further monitoring.
Surveillance of AMR contributes to the understanding of AMR situation and for monitoring the effectiveness of measures implemented. This surveillance exercise helps to contribute to the understanding of the AMR situation in Hong Kong.
AMR remains a serious threat in the world and Hong Kong is of no exception. Concerted efforts of different parties, including the prudent antimicrobial use and comprehensive infection prevention and control strategies, are the key measures to combat AMR.
Advice to the Public
- Proper use of antibiotics
- Do not demand antibiotics from your doctor
- Follow your doctor’s advice when taking antibiotics
- Do not stop taking antibiotics by yourselves even if you are feeling better
- Do not take leftover antibiotics
- Do not share your antibiotics with others
- Do not self-purchase antibiotics without a prescription
- Practise frequent hand hygiene, especially before eating and taking medicine, and after going to the toilet
- Ensure your vaccination is up-to-date
- Maintain cough etiquette, wear a surgical mask if you have respiratory symptoms
Advice to Healthcare Workers
Antibiotics are precious resources and their effectiveness must be preserved to protect us from infections. Healthcare workers play an essential role in preserving them:
- Prescribe antibiotics in accordance with therapeutic guidelines in consideration of clinical situations
- Educate your patients
- To take antibiotics as prescribed and always complete the full course of medication
- Discuss about the importance of appropriate antibiotic use and the dangers of AMR where appropriate
- Talk about how to prevent infections and their spread. For example, vaccination, maintain good personal hygiene and hand hygiene
- Apply best practice of infection prevention and control, and to practise frequent hand hygiene
- Receive seasonal influenza vaccine
Please click here to view the full report.
Please click here to view the previous reports.
Web accessibility conformance
We are committed to ensuring that our website conforms to the World Wide Web Consortium (W3C) Web Content Accessibility Guidelines (WCAG) 2.0 Level AA requirements to the maximum extent possible. However, as our website contains considerable tables and figures illustrating surveillance findings, it is not possible to incorporate all Level AA accessibility requirements in all of them. Please contact us by email at sp_icb@dh.gov.hk or by phone at 21252904. We will try our best to provide the information in a format accessible to you.
[1] The reference datetime is used to determine the display sequence of culture test report in IT systems of HA. The reference datetime is assigned according to the following rule: 1) Specimen collection datetime; 2) Specimen arrival datetime if 1) is not available; 3) Laboratory request registration datetime if 2) is not available.
[2] Episode number is a unique reference number assigned by each hospital to an episode of care. For an episode of care of inpatient nature, “HN” is assigned as the prefix of the episode number. For an episode of non-inpatient nature, other prefix is assigned as appropriate.
[3] The reference datetime is used to determine the display sequence of culture test report in IT systems of HA. The reference datetime is assigned according to the following rule: 1) Specimen collection datetime; 2) Specimen arrival datetime if 1) is not available; 3) Laboratory request registration datetime if 2) is not available.
[4] Episode number is a unique reference number assigned by each hospital to an episode of care. For an episode of care of inpatient nature, “HN” is assigned as the prefix of the episode number. For an episode of non-inpatient nature, other prefix is assigned as appropriate.
[5] Salmonella species and Streptococcus pneumoniae are pathogens primarily causing community-acquired infections. They are rare to cause hospital-associated infections. Information on location of onset is not considered when analysing and interpreting non-susceptibility results of these two pathogens. These results will be interpreted as isolates of undifferentiated location of onset.
[6] Rounded to the nearest thousand
[7] Rounded to the nearest thousand
[8] Non-susceptibility percentage (NS%) of amoxicillin/clavulanate for E. coli of community-onset ranged from the lowest 25.4% in year 2018 to the highest 32.5% in year 2013.
[9] NS% of amoxicillin/clavulanate for E. coli of hospital-onset ranged from the lowest 38.3% in year 2017 to the highest 47.1% in year 2013.
[10] NS% of piperacillin/tazobactam for E. coli of community-onset ranged from the lowest 3.7% in year 2018 to the highest 7.2% in year 2016.
[11] NS% of piperacillin/tazobactam for E. coli of hospital-onset ranged from the lowest 9.0% in year 2018 to the highest 15.1% in year 2012.
[12] NS% of gentamicin for E. coli of community-onset ranged from the lowest 28.2% in year 2018 to the highest 31.2% in year 2012.
[13] NS% of gentamicin for E. coli of hospital-onset ranged from the lowest 32.7% in year 2018 to the highest 39.5% in year 2012.
[14] NS% of amikacin for E. coli of community-onset ranged from the lowest 0.4% in year 2018 to the highest 1.4% in year 2013.
[15] NS% of amikacin for E. coli of hospital-onset ranged from the lowest 1.3% in year 2017 to the highest 3.1% in year 2012.
[16] NS% of cefuroxime for E. coli of hospital-onset ranged from the lowest 38.4% in year 2017 to the highest 48.6% in year 2012.
[17] NS% of cefotaxime for E. coli of hospital-onset ranged from the lowest 35.6% in year 2017 to the highest 44.4% in year 2012.
[18] NS% of ceftazidime for E. coli of hospital-onset ranged from the lowest 18.3% in year 2018 to the highest 27.2% in year 2012.
[19] NS% of levofloxacin for E. coli of hospital-onset ranged from the lowest 39.5% in year 2017 to the highest 49.7% in year 2013.
[20] NS% of cefepime for E. coli of community-onset ranged from the lowest 12.5% in year 2013 to the highest 24.0% in year 2015.
[21] Readers should take note of a new (revised) cefepime interpretive criterion for E. coli was released by Clinical Laboratory Standards Institute (CLSI) in year 2014, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility percentage.
[22] NS% of ciprofloxacin for K. pneumoniae of hospital-onset ranged from the lowest 18.4% in year 2012 to the highest 46.7% in year 2018.
[23] NS% of levofloxacin for K. pneumoniae of hospital-onset ranged from the lowest 12.8% in year 2012 to the highest 22.8% in year 2017.
[24] NS% of cefepime for K. pneumoniae of community-onset ranged from the lowest 4.8% in year 2012 to the highest 8.4% in year 2016.
[25] NS% of cefepime for K. pneumoniae of hospital-onset ranged from the lowest 9.3% in year 2013 to the highest 22.2% in year 2017.
[26] Readers should take note of a new (revised) cefepime interpretive criterion for K. pneumoniae was released by CLSI in year 2014, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility percentage.
[27] NS% of imipenem for K. pneumoniae of hospital-onset ranged from 0.5% in year 2017 to 3.2% in year 2018.
[28] NS% of meropenem for K. pneumoniae of hospital-onset ranged from 0.4% in year 2017 to 3.9% in year 2018.
[29] NS% of ampicillin for Salmonella spp. ranged from the lowest 35.0% in year 2012 to the highest 62.4% in year 2016.
[30] NS% of ciprofloxacin for Salmonella spp. ranged from the lowest 51.9% in year 2012 to the highest 76.4% in year 2017.
[31] Readers should take note of a new ciprofloxacin interpretive criterion for Salmonella spp. was released in year 2012, and modified recommendations to use the separate interpretive criteria were released by CLSI in year 2013, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility percentage.
[32] NS% of levofloxacin for Salmonella spp. ranged from the lowest 0% in year 2013 to the highest 86.4% in year 2017.
[33] Readers should take note of a new levofloxacin interpretive criterion for Salmonella spp. was released by CLSI in year 2013, which may be one of the contributing factors leading to the observed trend of respective non-susceptibility percentage.
[34] NS% of minocycline for Acinetobacter spp. of hospital-onset ranged from the lowest 18.9% in year 2018 to the highest 75.0% in year 2012.
[35] NS% of gentamicin for Acinetobacter spp. of hospital-onset ranged from the lowest 26.2% in year 2017 to the highest 50.3% in year 2013.
[36] NS% of amikacin for Acinetobacter spp. of hospital-onset ranged from the lowest 20.8% in year 2017 to the highest 40.7% in year 2013.
[37] NS% of co-trimoxazole for S. pneumoniae ranged from the lowest 47.0% in year 2013 to the highest 70.0% in year 2017.